The Clinical Playbook for Personalized Step-Down Programs that Prevent Readmissions and Improve Patient Outcome
From a hospital management perspective, our standard of care can no longer be confined to the physical walls of our building. The future of healthcare is about extending our clinical excellence into the community and the home. Our brand of care must follow the patient where they are.
This strategic shift is most critical in the 30 days after a patient leaves us.
This is the “post-discharge visibility gap.” It’s the period where our high-quality, in-patient care stops, and the patient is left on their own. For hospital leadership, this gap isn’t just a blind spot; it’s our single greatest point of unmanaged clinical risk and financial loss. It’s where preventable complications turn into high-cost emergency readmissions.
To solve this, we must extend our care. We must build a bridge over that 30-day gap.
The solution is a Personalized Digital Step-Down Program.
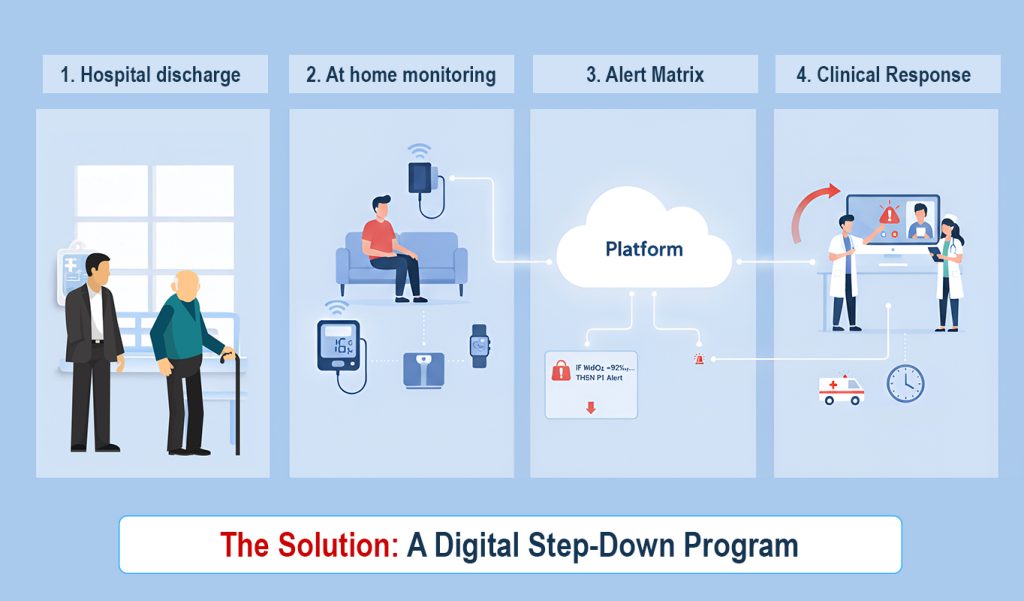
This is not a single product, but a flexible operational model. It uses a “Digital Backbone” platform to deliver custom care based on each patient’s unique clinical picture. This model is built on three pillars: Personalized Bundles, Personalized Alerts, and a Personalized Clinical Response.
Here is the in-depth playbook for designing one.
1. The Custom Device Bundle: Beyond “One-Size-Fits-All”
Many “RPM” solutions fail because they force a single device, like a BP cuff, on every patient. This “one-device” approach doesn’t do justice to the complexity of post-discharge care. A patient recovering from cardiac surgery has vastly different needs than one managing chronic COPD.
A truly effective program starts by creating specific “at-home kits” (device bundles) tailored to the patient’s condition. The kit must be simple for the patient: pre-configured, cellular-enabled, and ready to use right out of the box. The mix of devices, however, is a clinical decision.
Sample Device Bundles by Condition:

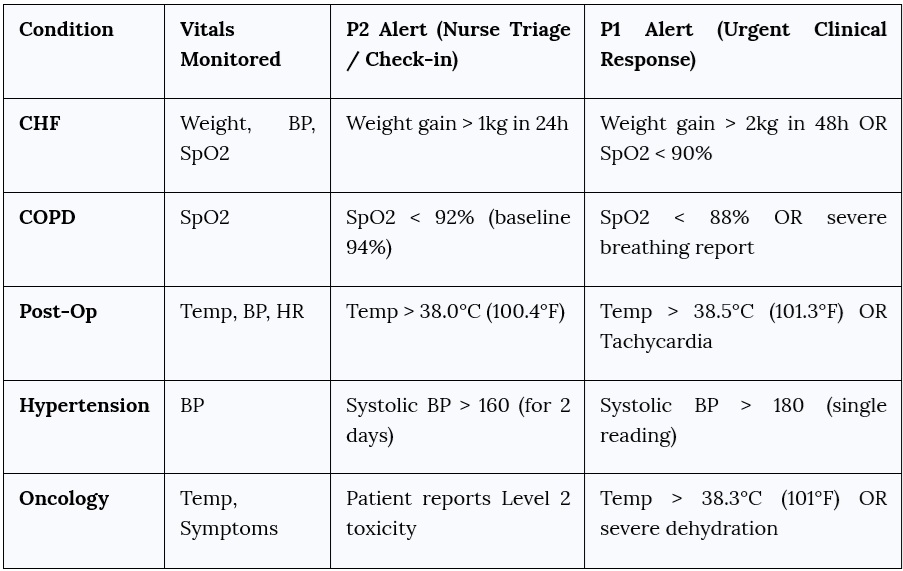
2. The Personalized Alert Matrix: The Clinician’s “Brain”
This is the “brain” of the platform. Raw data is just noise. A personalized alert matrix, set by your own clinicians, turns that noise into a clear, actionable signal.
Each patient is unique. A “normal” baseline for one patient may be a “high-alert” for another. A robust platform like MedTel’s allows your clinicians to set specific alert thresholds for each individual patient. This isn’t a “black box” algorithm; it’s your clinical expertise, scaled.
This clinical control is a critical management feature. It protects your most valuable asset—your staff’s time—from “alert fatigue” by filtering out irrelevant data.
Example Clinical Alert Matrix (Customizable per Patient):
3. The Personalized Clinical Response Workflow
The final piece is the operational workflow. The platform finds the problem; your team solves it. This response must also be personalized to be efficient.
Here’s how a robust workflow functions:
- Automated At-Home Monitoring: The MedTel platform automatically collects data from the patient’s device bundle. This can be fully automated (e.g., a weight scale) or caregiver-assisted. The platform filters 99% of the “normal” data, showing your nurses only the 1% of readings that fall outside the personalized rules.
- Clinician-Set Alerts: As shown in the matrix, your doctor sets the rules. This is the core of personalization. A frail elderly patient may have different “safe” thresholds than a younger patient recovering from the same surgery.
- Tiered Clinical Response: The response is not generic. It’s a clinical workflow that matches the severity of the alert, optimizing your staff’s time.
- Nurse-Led (P2 Alert): A P2 alert (e.g., moderate CHF weight gain) routes to the nursing team’s dashboard. This triggers a tele-consult to check medication adherence (“Did you take your diuretic?”), review diet, and provide patient education. Based on your hospital’s SOP, the nurse may even be authorized for a simple dose adjustment.
- Doctor-Led (P1 Alert): A P1 alert (e.g., severe SpO2 drop or chest pain) is a medical-grade event. It routes simultaneously to the nurse and the on-call doctor or specialist. This triggers an immediate clinical intervention, a STAT video consult with the doctor, or an urgent (but controlled) admission that bypasses the chaotic emergency room.
Case Study in Action: A Hospital Client During COVID-19
This personalized model was pressure-tested during the pandemic. One of our hospital clients needed to discharge stable COVID patients to free up beds, but couldn’t risk sending them home with no visibility.
- The Solution: We deployed a “Digital Step-Down” program in under 48 hours.
- Device Bundle: The “kit” was personalized based on co-morbidities. The standard bundle included a Pulse Oximeter and Thermometer. Patients with diabetes also received a Glucometer, while those with hypertension also received a Blood Pressure Monitor. This ensured we were monitoring not just the virus, but its impact on their chronic conditions.
- Alert Matrix: The primary life-saving rule was simple: Alert if SpO2 < 93%. Additional rules were set for high fever and, for diabetic patients, dangerously high glucose readings.
- Clinical Response: A dedicated nursing team monitored the central dashboard 24/7. When any alert triggered, they immediately launched a video tele-consult to assess the patient. This simple “Bundle + Alert” system allowed them to safely monitor hundreds of patients at home, save countless lives by catching “silent hypoxia,” and keep their critical ICU beds free.
This is the power of a true “Digital Backbone.” It’s not a rigid product. It’s a flexible platform that gives you the tools—custom bundles, personalized alerts, and tiered workflows—to design the exact program your patients and clinicians need.
This is how you extend your hospital’s standard of care beyond its walls.
Ready to design your hospital’s personalized step-down program?
Book a demo, and we will help you build the custom alert matrix and workflows for your highest-risk patients.