Humanizing Healthcare: Reshaping Patient Care Through Digitization
Overview
Overview
With increasing discussion about the digitization of healthcare and how healthcare and how the healthcare industry is ready for disruption and transformation, there is too much said and too little done at scale. This changed last year when due to the pandemic, healthcare professionals and patients had no option but to switch to teleconsultations and virtual care.
While this did help all the stakeholders, that is, the providers, payers, and patients get past their inertia of adoption to digital healthcare, it is a very interesting time to now leverage this momentum to push at-home digital healthcare from the early adoption phase to the early majority phase and also observe how sticky this switch can be!
Why Focus on Patient-Centric Care and What Would It Look Like?
Patients, especially chronically ill, need to be monitored regularly so that trends in their vital measurements can be studied and complications can be detected on time or even prevented in some cases. This increases their frequency of visits to the doctor and makes healthcare less proactive. Along with this, lifestyle changes become a huge part of patient treatment, and in a lot of cases patients are not as careful about their daily routines of exercises, medications, tests, and diet as they should be and they need subtle reminders to help them stay on track.
Remote Patient Monitoring (RPM)
The premise is that, the more a patient is involved in his/her healthcare, the healthier they will be. This helps the healthcare provider(s) and the patient to collaboratively handle the patient’s healthcare outcomes and makes the patients feel more confident about their situation.
Home Care
How do stakeholders benefit from digitization?
1. Personalization:- In the past, there have been massive efforts to make healthcare generalized so that the scope of error reduces. But we have realized that healthcare does not follow the one size fits all approach. Personalization has existed in theory, for quite a while now, but tailoring different approaches for different patients has challenges of its own. One of which is data and its aggregation to get useful insights. By digitizing healthcare, it becomes much easier to personalize treatments because the barrier of data collection and aggregation is automated. Healthcare providers can intervene with their expertise, deduce insights and ensure the best patient experience.
2. Faster and more accurate diagnosis of complications:- Since monitoring is done constantly in these approaches, any spike or dip in measurements would be tracked and trigger an automated alert to aid the healthcare providers in prioritizing and taking action at the earliest. Moreover, these channels give patients more options to be better connected with their doctors, which also ensures that all the warning signs are reported or detected. This ensures faster and more data-backed decision-making by healthcare providers.
3. Control misinformation:- With increasing internet accessibility and interest, patients usually resort to the internet to learn more about their condition. This not only negatively affects the patient who then worries about the worst-case scenario, but it also makes the doctor’s job difficult. Onboarding patients onto one platform which they can come back to, for all their healthcare needs, from prescriptions and consultations to learn about their condition, would help control misinformation and make sure that patients don’t walk in with a made-up diagnosis.
4. Shift healthcare from event-based to routine life:- In an RPM setup, a patient is more involved in his/her healthcare. This paired with personalized nudges to keep the patient motivated to stick to the lifestyle changes necessary to stay healthy and Minimize risk makes patients proactive and not wait for an emergency to begin to take action.
Roadblocks to digitization
While there are a lot of advantages to digitization and getting healthcare at home, there are some significant hurdles we need to cross to get there:-
1. Difference between data and insights: Data without context is an easy way to arrive at painstakingly wrong conclusions. The main problem here is that the context of the patient’s condition and lifestyle is best known by patients themselves and their doctors, data should be treated as a means to help the end goal of decision making in the patient treatment plans and not as a non-negotiable guideline.
2. The Chicken-egg problem: The barrier to adoption exists largely because there is still not enough evidence to support the hypothesis that digitizing healthcare would actually improve patient experience and healthcare outcomes. We need adoption first to be able to show outcomes, and we need outcomes in order to increase adoption. This loops us in a tricky matrix, breaking which would need smaller integrations with the traditional healthcare setup to build trust and understand the complexities of such solutions.
3. Healthcare providers believe it will add to their work: While building digital solutions for the healthcare ecosystem, it is very important to remember that a lot of times the end-user is not just the patient but also the healthcare provider(s). The best way to ensure that these solutions factor in all the stakeholders is to carefully consider what should be automated and what should not, and make sure that technology is used to tighten the loose ends of the traditional healthcare system and not replace it altogether.
4. Fear of inequitable access: In developing nations, with a split between people who can afford and have access to technology and those who can’t, there is some fear that approaches like remote patient monitoring can create a two-tier system and make healthcare inaccessible for a significant number of people. Introducing home care, or a one-to-many model at such places, would help bridge gaps between the tiers and make healthcare more accessible to everybody in one form or another.
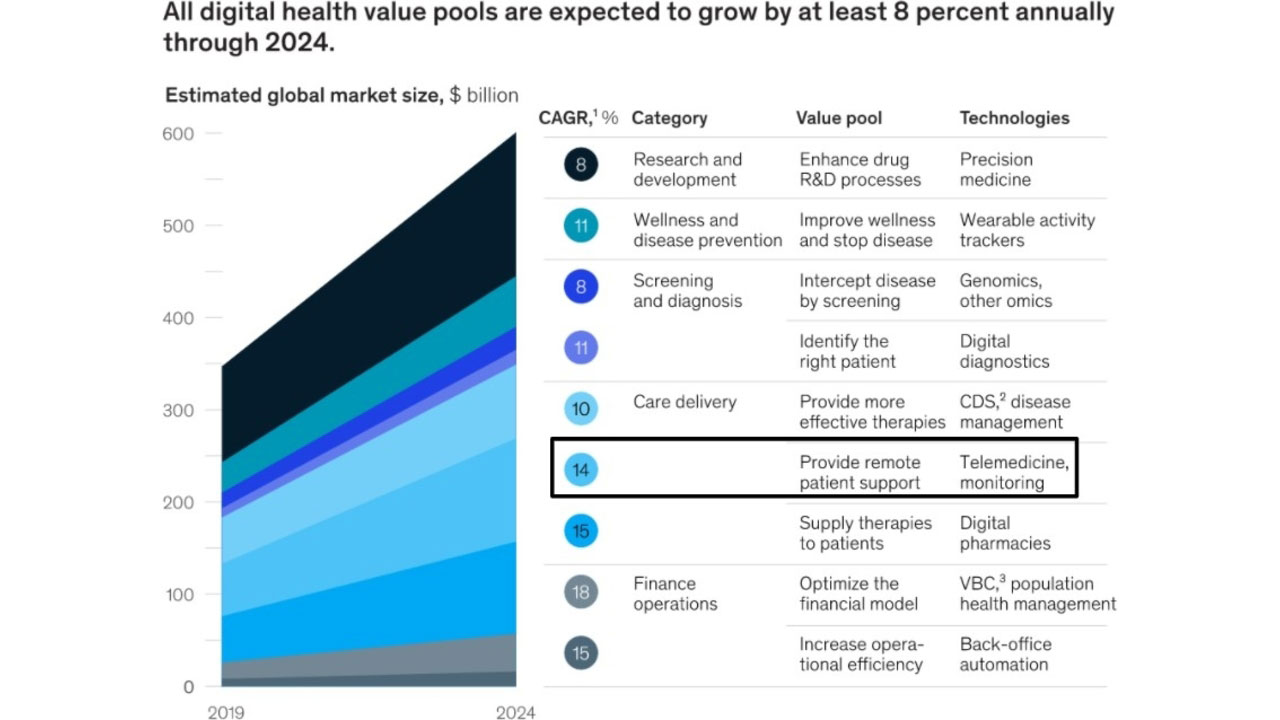
Why is now the right time to build a solution?
Along with this, the increasing investments in healthcare in the previous year have given a huge push to the innovations and experimentation in this domain. While these 2 factors have started the early adoption phase, it is now very crucial for all stakeholders of the ecosystem and digital healthcare companies to keep the ball rolling by understanding how to cross the next barrier, that is, keeping all stakeholders engaged and retaining the adoption so far while scaling the existing solutions.
Way Forward!
Way Forward!
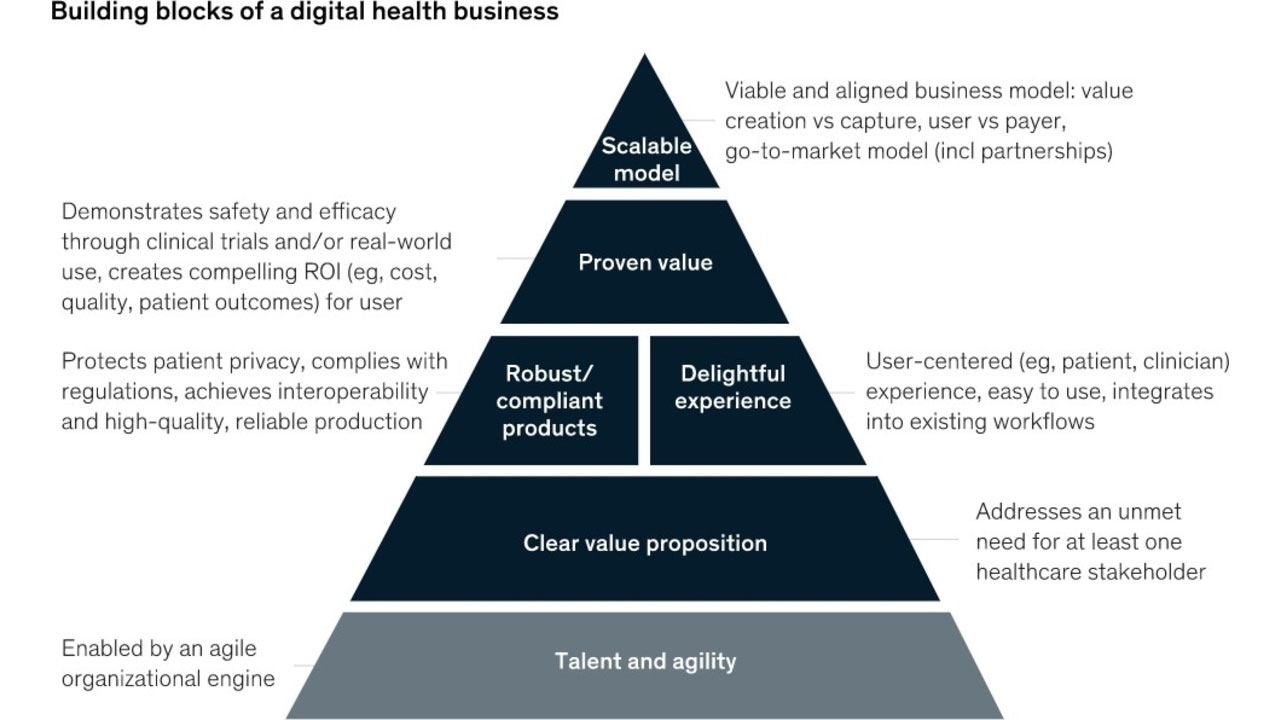
To make sure technology is used to solve a real problem and this doesn’t become just one more idea “ahead of its time” it is very important to let patients and doctors drive this change. Where and in what cases to use such interventions and how often, cannot be standardized and packaged as a one-size-fits-all.
Technology should be used to improve the shortcomings and pain points of the traditional healthcare systems and blend the old, new, and evolving to arrive at solutions that keep in mind the providers, payers, and the patients.
Contact Us!
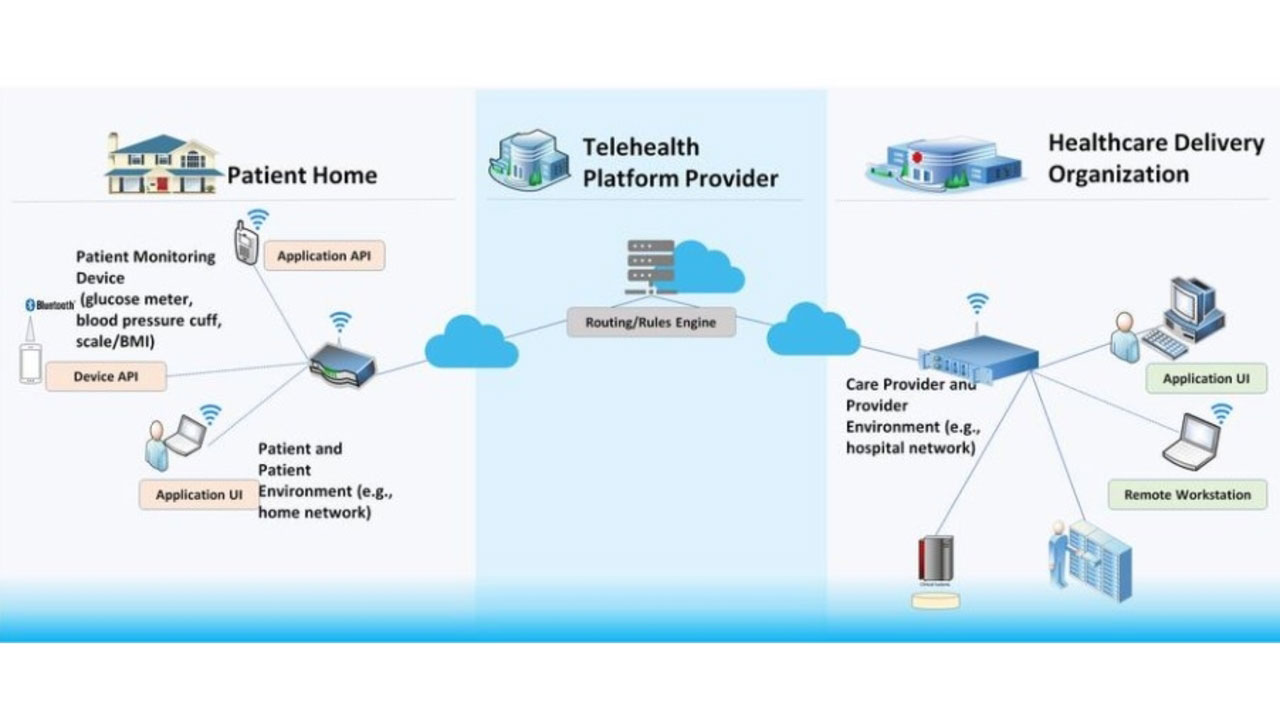
MedTel’s iRPM (one-to-one) and iLAB (one-to-many) platforms incorporate connected diagnostic devices, a smartphone app, and a web-based dashboard for hospital access and review. These devices include a digital blood pressure machine, body composition monitor, glucometer, Lipid profile, HbA1C, ECG, Otoscope, Fundoscopy, Urine dipstick, fetal heart rate monitor, and hemoglobinometer. Our advanced Connected Care Solutions provide remote care for hypertension, diabetes, pregnancy, and COVID. We also provide solutions for population health screening.